The 3 AM Club: You Are Not Alone
It’s 2 AM, then 3 AM… The ticking of the clock sounds deafeningly loud in the silence. Thoughts like “I have a meeting at 9 AM,” or “If I fall asleep right now, I’ll get exactly 4 hours of sleep,” start to race through your mind. Ironically, the harder you try to force yourself to sleep, the more awake you become.

Insomnia is one of the most common health complaints in modern society. It’s not just about “not sleeping”; it ruins your next day, kills your productivity, and long-term deprivation threatens your immune system and mental health.
Today, as a health curator who digs deep into medical data, I want to share a guide that goes beyond generic advice like “drink warm milk.” We are going to look at evidence-based strategies to fix your broken sleep cycle.
Let’s end the struggle tonight.
1. Why Can’t I Sleep? (The Mechanism of Insomnia)
To understand why you’re awake, you need to understand the two systems that control sleep: Sleep Pressure and Circadian Rhythm.
1) Adenosine and Sleep Pressure
While you are awake, your brain accumulates a chemical called Adenosine. Think of this as “sleep hunger.” As it builds up throughout the day, it creates “sleep pressure,” signaling your body that it’s time to rest. However, if you nap too long during the day or are completely sedentary, this pressure doesn’t build up enough, leaving you wide awake at bedtime.
2) The Battle: Melatonin vs. Cortisol
At night, your pineal gland should release Melatonin (the vampire hormone that comes out in the dark). But modern life is too bright. Blue light from smartphones tricks your brain into thinking it’s still daytime, suppressing melatonin. Conversely, chronic stress keeps Cortisol (the arousal hormone) levels high at night, putting your body in “fight or flight” mode rather than “rest and digest.”
When these rhythms are out of sync, even if you do sleep, you miss out on deep restorative sleep, leading to that “tired but wired” feeling.
2. Do I Have Insomnia? (Symptoms & Self-Check)
Many people think you have to pull an all-nighter to call it insomnia. However, medically, it manifests in different ways.
- Sleep Onset Insomnia: You struggle to fall asleep for more than 30 minutes. (Most common).
- Sleep Maintenance Insomnia: You fall asleep but wake up frequently (2+ times) or struggle to fall back asleep.
- Early Morning Awakening: You wake up way too early (e.g., 4 AM) and can’t sleep again.
The Self-Checklist
If you check 3 or more of the following, and this happens at least 3 nights a week for over 3 months, you may be dealing with chronic insomnia.
- My mind races with worries as soon as my head hits the pillow.
- If I wake up in the middle of the night, it takes ages to sleep again.
- I wake up feeling unrefreshed, heavy, or irritable.
- I start dreading bedtime (“Will I sleep tonight?”) as evening approaches.
- Daytime fatigue or brain fog affects my work or relationships.
3. How Is It Diagnosed?
“Do I really need a doctor for this?” If it’s chronic, yes. Getting a professional assessment can rule out hidden issues.
- Polysomnography (Sleep Study): This is the gold standard. You spend a night at a clinic while they monitor your brain waves, oxygen levels, heart rate, and limb movements. It helps rule out Sleep Apnea or Restless Legs Syndrome.
- Sleep Diary: Doctors often ask for this first. You record your bedtime, wake time, caffeine intake, and naps for about two weeks to find patterns you might have missed.
4. How to Sleep Without Pills: CBT-I and Lifestyle Hacks
Sleeping pills are like a fire extinguisher—good for emergencies, but they don’t prevent the fire from starting again. Major health organizations, including the American Academy of Sleep Medicine, recommend CBT-I (Cognitive Behavioral Therapy for Insomnia) as the first-line treatment, not medication.
Here are the core CBT-I techniques you can try at home.

1) Stimulus Control (Crucial!)
You need to re-train your brain to associate the bed only with sleep.
- Go to bed only when sleepy: Not just because it’s 11 PM. Wait for the “heavy eyelids” feeling.
- The 15-Minute Rule: If you haven’t fallen asleep within roughly 15-20 minutes, get out of bed. Go to another room, read a dull book, or meditate. Only return when you are sleepy. Lying there awake trains your brain to link the bed with anxiety.
- No activities in bed: No TV, no eating, and absolutely no work or phone scrolling in bed.
2) Sleep Restriction Therapy
It sounds counterintuitive, but limiting your time in bed can improve sleep efficiency.
- If you only actually sleep 5 hours a night but lie in bed for 8 hours, you restrict your “time in bed” to closer to 5.5 hours initially. This increases sleep pressure, making you fall asleep faster. (Note: Consult a professional before trying this strictly).
3) Sleep Hygiene Upgrade
- Total Darkness: Invest in blackout curtains. Even a sliver of street light can disrupt hormones.
- Temperature Drop: A warm shower 1-2 hours before bed helps. As your body cools down post-shower, it signals the brain that it’s time to sleep.
- Caffeine Curfew: Caffeine stays in your system longer than you think (half-life of 5-6 hours). Try to stop all caffeine intake after 2 PM.
5. When to See a Doctor
Sometimes, insomnia is a symptom of something else. Please consult a healthcare provider if:
- Snoring or Gasping: If you snore loudly or stop breathing during sleep, it could be Sleep Apnea, which increases the risk of cardiovascular disease.
- Restless Legs: An uncomfortable crawling sensation in your legs that makes you want to move them (Restless Legs Syndrome).
- Mental Health: If anxiety or depression is the root cause, treating the sleep issue alone won’t work.
- Pill Dependency: Over-the-counter sleep aids or prescription drugs can lead to tolerance. If you feel you “can’t function” without them, seek medical help to taper off safely.
Editor’s Note: Medication should generally be a short-term solution under a doctor’s supervision. Don’t let a temporary crutch become a permanent necessity.
6. Stop Chasing Sleep
The biggest secret to overcoming insomnia is learning to let go. The anxiety of “I must sleep” is often the very thing keeping you awake. Adopting a mindset of “If I don’t sleep well tonight, I’ll just be a bit tired tomorrow, and that’s okay” can paradoxically help you relax enough to drift off.
Start small tonight. Charge your phone outside the bedroom and apply the 15-minute rule. It takes time to reset a biological clock, but your body knows how to sleep; you just need to get out of its way.
Here’s to a peaceful night’s rest.
FAQ: Frequently Asked Questions
Q1. Does a “nightcap” (alcohol) help with sleep?
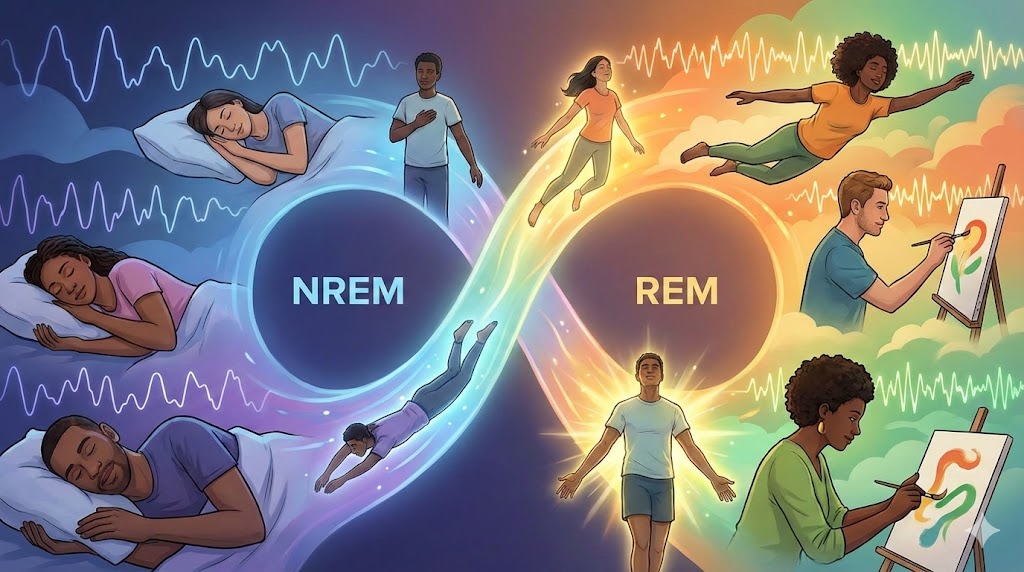
A. It’s a common myth. While alcohol acts as a sedative and helps you fall asleep faster (onset), it severely disrupts REM sleep and sleep architecture. This leads to fragmented sleep, frequent waking, and feeling groggy the next day. It is not a sustainable sleep aid.
Q2. Are Melatonin supplements safe?
A. Melatonin can be helpful for circadian rhythm disorders (like jet lag or shift work), but it is not a cure-all for chronic insomnia. In some countries, it is over-the-counter; in others, prescription-only. Dosage varies widely, so consult a doctor before long-term use.
Q3. Can I catch up on lost sleep during the weekend?
A. Be careful of “Social Jetlag.” Sleeping in too late on weekends can push your body clock back, making it impossible to fall asleep on Sunday night and worsening the “Monday Blues.” Try to keep your wake-up time within 1-2 hours of your weekday schedule.
[Related Articles & Internal Links]
- “Natural Supplements for Stress: Magnesium Guide” [LINK]
[Disclaimer] The content provided in this article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The causes and symptoms of insomnia can vary by individual. Always seek the advice of a physician or other qualified health provider with any questions you may have regarding a medical condition.
